Population Health Academy Newsletter
Prevention and Inequalities Regional Updates
Publications and guidance
- The HIV Action Plan for England has been published, setting out how the government will reach its ambition of ending new HIV transmissions by 2030.
- The Department for Health and Social Care clinical guidelines for alcohol treatment provides a clear framework for improving consistency and quality of care. The guidelines emphasise the role for mandatory alcohol screening in acute hospitals and specialist alcohol care teams in delivering evidence-based interventions.
Prevention
- Short summary of the data updates to OHID’s Mortality and Alcohol profiles on Fingertips.
- CVDPrevent 2025 Annual Audit Report has now been published. The report summarises key national findings and recommendations from the March 2025 core data and January 2024 – December 2024 outcomes data.
- There is an infographic which details key findings on hypertension, cholesterol and chronic kidney disease as well as the findings from the patient and public report for March 2025 and outcomes indicators guidance.
- Visit the DHSC Campaign Resource Centre for more information about ongoing New Year campaigns, NHS Healthy Choices Quiz and New Year 2025/26 Quit Smoking.
Health inequalities
- Health Information Week (19- 25 January 2026) which provides an opportunity to promote the NHS App. Resources and assets available.
- Reminder about NHS England's Ethnicity Recording Improvement plan.
- Recording of the recent webinar about the plan is available on the FutureNHS platform. The webinar covers the ambitions and expectations relating to the plan as well as providing some practical examples.
- Office for National Statistics (ONS) has published subnational trends in period life expectancy between 2001 to 2003 and 2022 to 2024.
- The Inclusion Health Dashboard was published on the 8th January 2026. This new interactive national resource has been a collaborative project between DHSC OHID, UKHSA, NHSE with representatives from local government, ICBs and VCSE. It aims to support work on inclusion health at a local level. The dashboard contains information on:
- People experiencing homelessness
- Gypsy, Roma and Traveller communities
- Sex workers
- Migrants in vulnerable circumstances
- People subject to modern slavery
- People in contact with the justice system
- People experiencing drug and/or alcohol dependence
Training, learning opportunities and events
- OHID colleagues are currently running webinars on Fingertips:
- Fingertips Plus – 21st January 2026 @ 10:30am -12:30pm
- Intro to Fingertips - 12th February 2026 @ 1:30 - 3:00pm
- North East and Yorkshire team have shared resources relating to Tobacco Dependency Services, specific highlights include:
- There will be a CVDPREVENT webinar on their findings and how you can use the data to inform quality improvement
- Thursday 12th February 2026 @ 2pm – 3pm
- To register, enter your details here.
- If there is any feedback on outputs or for any other queries, please email nhsbn.cvdprevent@nhs.net
- NHSE SE Region are hosting the following meetings in the coming months:
- DWMP Lunch and Learn – 21st January @12:30-13:30 (online)
- The session is for colleagues working in general practice, who can register here. Please share with relevant colleagues/networks.
- Tobacco Community of Practice – 19th February @ 11:00-12:00 (online).
- If you would like an invite, please email ben.crawford1@nhs.net or lewis.clarke@nhs.net
- DWMP Lunch and Learn – 21st January @12:30-13:30 (online)
- Introduction to the Model Health System Webinar
- Thursday 15th January @ 11:30 - 12:30 (Online)
- This session will help you to:
- Log in and navigate the system
- Find the data you're looking for
- Understand the range of graphs and charts
- Download your data
- Identify areas of opportunity
- Register here
- You will also hear about the latest updates, features, and developments and have the opportunity to ask questions to the panel of speakers.
- The Health Foundation are hosting a webinar on inclusive growth and healthy places, which will be showcasing good practice in how to deliver local growth and improve health
- 28th January 2026 @12:15
new guidance on tobacco dependence treatment for people with severe mental illness.Publications and guidance
- The Department of Health and Social Care (DHSC) have recently published a policy paper on a Men’s Health Strategy for England, which is accompanied by an equality impact assessment.
- Please follow the link for the Keep Britain Working Review, which is an independent review of the role of employers play in tackling health based economic inactivity and promoting healthy and inclusive workplaces.
- Recommendations and actions as a result include launching an employer vanguard programme, a Healthy Workplace Standard, creating a workplace health intelligence unit.
- The Strategic commissioning framework sets out what NHS England expects from ICBs in the strategic commissioning role, and what ICBs and providers can expect from NHS England.
- Key data publications:
- The Chief Medical Officer has published their report on health trends and variation in England 2025, which gives an overview of the health of England’s population, including trends over time and geographical variation.
- The Segment Tool has been updated to include data from the 2022-23 period. A short briefing note can also be found attached, which provides information on the causes of death and age groups that are driving inequalities in life expectancy at a local level.
- The National Child Measurement Programme (NCMP) annual report for the 2024/25 academic year is now available. This reports details patterns and trends in child body mass index category for children in reception and year 6. Headlines for the South East include:
- Regionally and nationally, we have seen significant increases in prevalence of obesity among reception children in 2024/25 compared to 2022/23.
- Obesity prevalence in year 6 remains similar to last year
- Large inequalities still exist, with children living in the most deprived areas more than twice as likely to be living with obesity and up to four times more likely to be living with severe obesity compared to those living in the least deprived areas.
- An interactive report, the Health of the Region data explorer, has been launched to support comparison of a range of public health indicators across England’s 9 regions and their local authorities.
Prevention
- The Office for National Statistics (ONS) have released updated data on adult smoking habits in the UK. This includes how many people smoke, differences between population groups, changes over time and use of e-cigarettes.
- The Smoking Profile on Fingertips was also updated in November. This included updates to prevalence by occupation and by presence of mental health condition as well as several updates to stop smoking service data indicators.
- Following ONS revisions to the source data, indicators based on single year APS between 2020 and 2023 have been revised. Indicators based on the 3-year APS for 2020 to 2022 and 2021 to 2023 will be revised at a future Fingertips update.
- There has been an update to ASH’s Tobacco Dependency Treatment service impact calculator. Full details of the update can be found on the “about” tab.
- There have been a couple of insightful reports relating to alcohol consumption. One from the Institute for Public Policy Research on counting the economic costs of alcohol harm and the other from the Institute for Alcohol Studies which sets out a long-term vision to tackle alcohol harm in the UK and includes key targets and policy recommendations.
- The NCSCT have published new guidance on tobacco dependence treatment for people with severe mental illness.
- ONS have published modelled estimates relating to the relationship between the NHS Diabetes Prevention Programme and monthly earnings, employee status and unplanned hospital admissions in England
- Current health and social care committee inquiries are hearing oral evidence:
- Healthy Choices Quiz launched on 4 November 2025. The quiz asks a series of questions about users’ lifestyles, including movement, eating, alcohol consumption, smoking and vaping, mental health and sleep. Users then receive an overall score out of 10 based on their answers, personalised recommendations and links to NHS resources. Download the campaign toolkit here.
- The ‘Let’s Move!’ campaign launched on 2 Nov 2025 to keep families active all year around.
Health inequalities
- Reminder that the NHS Race and Health Observatory (NHS RHO) have developed the Health Action Resource Platform (HARP), which allows users to explore NHS performance data broken down by ethnicity across regions, systems and providers. It aims to illustrate racial inequalities in heath through data visualisation.
- Research and analysis from the Chief Medical Officer for England identifies areas of good practice and areas of risk in relation to the health of people in prison, on probation and in the secure NHS estate in England
- NHS England has collaborated with NHS Confederation to develop the Health Inequality Assurance Framework, which is a self-assessment improvement tool for Integrated Care Boards (ICBs). The tool is designed to support ICBs in assessing progress on tackling health inequalities in relation to strategic objectives and commissioning plans.
- NHS England have also recently published a refreshed Statement on information on health inequalities, which relates to legal duties under section 13SA of the National Health Service Act 2006. Some highlights include:
- Building on the 10 Year Health Plan, the publication sets expectations for how NHS organisations should adopt a transparent and evidence-led improvement approach to tackling health inequalities, in line with Core20PLUS5.
- In annual reports, ICBs, trusts and foundation trusts must review the extent to which it has met NHS England's views set out in the statement.
- The statement should also support ICBs to meet the Medium Term Planning Framework ask to demonstrate how they will reduce health inequalities in the exercising of their functions.
- Data on Physical Health Checks for People with Severe Mental Illness in Q2 2025/26 is now available.
Training, learning opportunities and events
- NHSE SE Region Prevention and Healthcare Inequalities Team is hosting another Lunch and Learn for the Digital Weight Management Programme (DWMP)
- 21st January 2026 @ 12:30 – 13:30 (online)
- The session is primarily for colleagues working in general practice to support their understanding of the programme, how to refer and how it can benefit their populations
- Please share the registration link with relevant general practice colleagues in your network
Other useful links
- A new report from The RSPH examines the health outcomes of adults using social care services and how the social care system can have a more active role in health improvement.
- The Local Government Association (LGA) Inform and the Centre for Ageing Better have produced a new tool that gives a snapshot report of key data available at the local authority level to help local councils to better understand their ageing population and support better planning and service delivery
- UKHSA has shared research and analysis on how climate change and mental health are interlinked. The link includes a summary for policymakers.
Publications and guidance:
- NHS England have published the Medium Term Planning Framework to support planning across Systems.
- The Tobacco and Vapes Bill is currently being considered by parliament. Whilst there is good evidence for policy in several areas, there are some topics that further evidence is being sought. As such, there is a call for evidence currently open that runs until 3rd December 2025.
- NHS England are in the process of rolling out a new long-acting injection for people at risk of HIV but unable to take pre-exposure prophylaxis (PrEP) tablets. Read more about it here.
- Statistics on the English indices of deprivation 2025 have been released which provide an update to the English indices of deprivation 2019. This also includes various summaries (for example, ICB summaries).
- National Centre for Smoking Cessation and Training (NCSCT) have shared guidance around tobacco dependence treatment for people with severe mental illness with best practice recommendations and guiding principles that have been drawn from published literature and clinical experience.
- The Chartered Institute of Public Finance and Accountancy (CIPFA) have published a report on investing in prevention that offers a practical step-by-step guide for public sector organisations to map and measure preventative spend and investment.
- NHS England has published a request for action on racism including antisemitism. The request is aimed at System partners in implementing initiatives that support our shared committed to fostering an inclusive, respectful and professional environment for everyone.
- The Office for Health Improvement and Disparities (OHID) have released guidance on promoting work as a health outcome for Allied Health Professional leaders.
Prevention:
- West Yorkshire Health and Care Partnership have published a report exploring the human, social and economic cost of obesity for the West Yorkshire, Humber and North Yorkshire ICB populations. The 'More Than Weight: Exploring the human, social and economic cost of obesity' report contains recommendations and infographics as well as the research methodology that went into pulling it together.
- The SE region Prevention and Healthcare Inequalities team hosted a regional Tobacco Community of Practice event on the 16th October. The session had a focus on pharmacotherapy. The recording along with resources can be found here.
- Several Tobacco related resources have been added to Future NHS this month. They are summarised for convenience here:
- Presentations delivered at the National Smoking in Pregnancy Community of Practice, Inpatient tobacco dependence: Physical acute peer support session and Mental Health Inpatient Tobacco Dependence Peer Support Session have been uploaded and can now be sorted by name which will show all recent additions at the top.
- The World Health Organisation (WHO) have released a report on global trends in prevalence of tobacco use 2000–2024 and projections 2025–2030.
- Alcohol Change UK have shared findings from an evaluation conducted by Buckinghamshire Council’s Blue Light Approach, which aims to better support those living with severe alcohol dependence.
- The Scottish Government has released data that shows the number of alcohol specific deaths to have fallen by 7% in Scotland to 1,185 in 2024. The data has been contextualised with some of the policy decisions that may have led to this decrease.
- NHS England has published the latest Statistics on Local Stop Smoking Services in England - April 2025 to June 2025 (Q1).
- The Smoking Profile on Fingertips has been updated for October 2025 including 3 indicators about smoking quitters:
- National colleagues have shared an evidence pack with slides aimed at supporting commissioners, regional leads and other colleagues working on tobacco dependence to help set out how the current NHS priorities and strategic drivers can be realised through delivery of tobacco dependence treatment services.
Health inequalities:
- The Department of Health and Social Care (DHSC) has issued a press release around the review of the GP funding formula, which is expected to deliver fairer distribution of funding and address health inequalities.
- TransActual have published a report on UK Healthcare Worker’s experiences, confidence and comfort supporting trans patients
- Highlighting the Health Inequalities Improvement Programme page on the FutureNHS platform that is dedicated to tools and resources relating to the Core20 most deprived population. This ranges from guidance, tools, research and reports and includes ICS Deprivation Heat Maps, which may be of use to colleagues.
- As part of ongoing work to improve ethnicity recording, there are several case studies available on the FutureNHS platform on work that has been done in this area: Case Studies - Improving Ethnicity Recording
- The Health Anchors Learning Network have shared the work going on in Suffolk and North East Essex ICS in creating a system-wide approach to anchor impact measurement
- A rapid read for staff working with young people who are seeking asylum. This has been developed following concerns shared in region and from other regions about the use of medicines by these young people. Input was sough from a wide range of colleagues including Regional Controlled Drugs Officer, Designated Doctors and Nurses, Migration Partnership Principal Social Worker, Barnardo’s, Home Office accommodation provider safeguarding leads, Public Health Consultants and substance use experts.
Training, learning opportunities and events:
- Resources and training are available via the Futures NHS Platform from The Faculty for Value Based Care. These resources provides health and care leaders with insight, resources and learning to better understand and implement ‘value-based care’ in their roles. The work has been supported by Sir Muir Gray and by learning from the Oxford Value and Stewardship Programme, offering information and tools to support leaders to champion a culture of stewardship, drive allocative efficiency, and minimise waste across the NHS.
- Webinar: Addressing Health Inequalities for Women on Probation
- 25 November @ 12:00 – 13:30 (online)
- This webinar will give clinical insights and real-world perspectives as well as offering an opportunity for reflective practice and finding collaborative solutions.
- Registration and further details can be found here
- Webinar: Celebrating success: one year of the National Smoke-free Pregnancy Incentives Scheme
- 26 November @ 10am – 11:30am (online)
- This event is for anyone involved in or supporting delivery of the scheme
- Registration and more details can be found here
- The Health Foundation are hosting some webinars that may be of interest:
- Driving better health through English devolution, which will bring together colleagues from strategic authorities and their partners from across England to explore how regional leadership can drive better health outcomes - Wednesday 5 November 2025, 10.00–16.00 - Free, in-person event, Register here
- Understanding preventative investment: how to map and measure spend, with the Chartered Institute of Public Finance and Accountancy (CIPFA) for the launch of its report on preventative investment in local government - Thursday 6 November 2025, 13.30–14.30 - Free, in-person event, Book now
- The South East Health Innovation Networks are hosting a series of webinars on different aspects of heart failure between September and November. Registrations are still open, links below:
- Heart Failure: Frailty/End of Life and HF in Younger Patients - 27 November, 12pm – 1pm (online) - Register here
- OHID colleagues are hosting further webinars as part of their Public Health Intelligence webinar series:
- Fingertips Plus - 18th November 2025 @ 1:30pm-3pm (online)
- PHI/Exchange – 19th November 2025 @10 am – 12:30pm (online)
- Introduction to Fingertips – 10th December 2025 @ 1:30pm-3pm (online)
Other useful links:
- Call for evidence outcome around the National TB action plan has been published (current 2021-2026 here: Tuberculosis (TB): action plan for England
- The Local Knowledge and Intelligence Service evaluation framework has recently been launched on PHI/Online. The framework has been designed to help plan evaluation of intelligence outputs, but also provides general guidance on evaluation. You can take a look at the framework in our PHI/Online Resources section. The framework also includes a Discussion Forum for you to post any questions on evaluation, along with a Resource Library, which we are hoping will develop into a useful resource with guidance and examples of evaluation. If you have any queries about the framework, please contact LKIS@dhsc.gov.uk. (Announcement: launch of new evaluation framework for intelligence outputs - Public Health Intelligence Online - Futures)
Prevention and Inequalities National Updates
A message from Dr Dianne Addei, Director - National Healthcare Inequalities Improvement Programme, NHS England
As we come to the end of 2025, I wanted to reflect on a year that has filled me with immense pride at the progress we have collectively made to further reduce health and healthcare inequalities.
The NHS England Healthcare Inequalities Improvement Programme has continued to set the direction for the healthcare system, and this year we launched several important resources to guide action on addressing inequalities.
In the Spring, our Community Language Translation and Interpreting Services framework was launched and will benefit people with limited English proficiency.
We also published the Patient Safety Healthcare Inequalities Reduction Framework, to set out principles to reduce patient safety healthcare inequalities in the NHS.
In June, I was delighted to see the renewed focus on inequalities at NHS ConfedExpo where, once again, there was a dedicated health inequalities learning theatre sharing exceptional examples of work from programmes and projects across England.
I’m very pleased to say that the Ethnicity Recording Improvement Plan we produced has been very well received by partners. It sets out targeted actions to strengthen the quality, consistency and completeness of ethnicity data recording in the NHS.
In November, NHS England’s statement on information on health inequalities was published to support relevant NHS bodies to fulfil their health inequalities legal duties.
One of my personal highlights this year has been travelling around the country to hear first-hand about the incredible work teams are doing. However, it has reminded me that, although we are fully committed to making great strides together, there is more work to be done for those who are disadvantaged.
Our work would not be possible without your tireless commitment, unwavering support and passion for tackling inequalities, so thank you for all that you have done this year to support those who are less privileged than us.
I wish you and your loved ones a very happy and healthy 2026.
With best wishes,
Dianne
Latest updates
Sheffield’s Sickle Cell Bypass Unit: improving urgent care and tackling inequalities
People with sickle cell disorder often face long waits in emergency departments before receiving the specialist care they need. Sheffield Teaching Hospitals NHS Foundation Trust is changing that with its innovative Sickle Cell Bypass Unit, allowing patients to bypass A&E and access expert treatment quickly.
The service supports over 700 patients across Yorkshire and the Northeast, reducing hospital stays and improving patient experience. Patients have 24/7 access to specialist care, making Sheffield one of a handful of centres nationally offering round-the-clock support, improving care for patients.
This work is part of NHS England’s commitment to tackling healthcare inequalities and improving outcomes for people with sickle cell and thalassaemia.
Read more about the unit here.
In photo: Dr Dianne Addei on a visit this month to the Sheffield Sickle Cell Bypass Unit at Royal Hallamshire Hospital.
Find out more about the visit and work of the unit
Understanding the sickle cell trait: why knowledge matters
Read Dr Layan Allawi’s new blog, Understanding Sickle Cell Trait: Why Knowledge Matters, to find out why it's important to know if you have sickle cell trait.
A free NHS genetic blood test – arranged through your GP practice – can tell if you have the sickle cell gene, says Dr Allawi, an NHS England Sickle Cell and Thalassaemia Clinical Fellow.
Co-creating the digital front door to the NHS
The NHS App enables millions of people to access essential healthcare services, but some risk being left behind due to barriers that limit their access or confidence in using it. In a new blog, user researchers Tanja Galloway, Lisa Collins and Simon Davis explore the experiences of people who are often underrepresented in digital health.
Through inclusive research and close partnerships with community organisations, they are helping shape improvements that make the app easier to navigate and more accessible for everyone.
Health improvement training for Core20PLUS Connectors
In collaboration with the Royal Society for Public Health, we are pleased to announce that 12 free places are now available on a new health improvement training programme for Core20PLUS Connectors working across England.
This is part of a wider collaborative strategy to develop the capacity and capability in communities to tackle inequalities and improve health and wellbeing.
Click here to find out more and apply. The deadline for applications is 30 January 2026.
News from our partners
Tackling HIV stigma
On World AIDS Day (1 December 2025), King's College Hospital NHS Foundation Trust launched a powerful new film challenging the stigma and community isolation that can come with a HIV diagnosis.
A Changing Landscape: from uncertainty to acceptance is a new mini-documentary, created by King’s and funded by Gilead Sciences. It features three south Londoners who share their personal experiences of living with HIV.
The film highlights the significant progress made in treatment and support, showing that individuals with HIV can lead long, healthy and thriving lives.
Be Epilepsy Aware – online version launched
Working in partnership with Epilepsy Action, The North East and Cumbria Learning Disability Network has launched a free online version of 'Be Epilepsy Aware'. This has been co-produced alongside people with a learning disability and has been developed to be an accessible epilepsy awareness course.
It provides accessible epilepsy awareness education to empower people with a learning disability to better understand and live well with epilepsy and to educate people who do not have epilepsy to better understand the condition and support those living with it.
The course is suitable for anyone who would like to learn more about epilepsy.
Birmingham Men’s Health Needs report
Read the recently-published Birmingham Men’s Health Needs Report, developed by Birmingham Inclusion Health in collaboration with partners across the city.
The report summarises the latest evidence on men’s health in Birmingham and identifies key drivers of premature mortality, including cancer, cardiovascular disease, mental health, lifestyle risks, substance misuse and health literacy. It provides strategic recommendations to help local systems reduce health inequalities through stronger prevention, early intervention and targeted support, aligning with many of the key levers outlined the new Men's Health Strategy for England.
NHS Race and Health Observatory announce exchange partnership in Brazil to advance global health equity
The NHS Race and Health Observatory (NHS RHO) has announced a landmark exchange partnership with SUS SUAS Sem Racismo (Health Without Racism) in Brazil to tackle racial inequalities in healthcare, representing a significant advancement in its global equity initiatives. The partnership is centred on collaborative learning regarding racial and ethnic health disparities, particularly concerning data ethics, inclusive workforce strategies and community engagement.
This collaboration will provide health inequalities improvement teams the opportunity to benchmark UK initiatives in an international context, enhancing the exchange of insights that strengthen local and global efforts toward equity. Read more from NHS RHO Chief Executive Professor Habib Naqvi.
Events and webinars
Join our Healthcare Inequalities Improvement Forum
Wednesday 21 January 2026 - 10:00 am - 11:30 am | Online
The Forum - which takes place monthly - is a national platform for health and social care professionals with a keen interest in reducing health inequalities, including colleagues working at regional and system levels in the NHS.
It aims to promote collaboration, facilitate shared learning and provide support across the NHS. It is instrumental in shaping health policy, identifying barriers, sharing good practice and enhancing the capacity of the system to achieve equitable health outcomes.
If you have any questions, please email england.healthinequalities@nhs.net
Book your place at NHS ConfedExpo 2026
Registration is now open for NHS ConfedExpo, the UK's leading health and care conference, returning to Manchester Central on 10-11 June 2026.
Connect with key decision makers, explore innovative ideas, and discover how teams are turning the ambitions of the 10 Year Health Plan into a reality.
If you have a bold idea, pioneering project, or practical insight to share, submit a breakout session proposal and be part of shaping the 2026 programme. Find out more about the submission process.
Book your place. NHS, local authority and public sector staff receive free tickets.
A message from Dr Dianne Addei, Director - National Healthcare Inequalities Improvement Programme, NHS England
This month, we published an updated Statement on Information on Health Inequalities, providing guidance on how NHS organisations should adopt a transparent and evidence-led improvement approach to tackling health inequalities, in line with Core20PLUS5.
The Medium Term Planning Framework asks NHS organisations to demonstrate how they will reduce health inequalities in the exercise of their functions. The statement supports this by setting out a description of the powers available to integrated care boards (ICBs) and NHS trusts to collect, analyse and publish information, and NHS England’s view about how these powers should be exercised to address health inequalities.
It includes specific expectations on how information should be used to identify population health needs, understand inequalities in access and outcomes, surface data quality issues, and inform targeted action.
We will be hosting a webinar on the updated statement from 11:00 am - 12:00 pm on 13 January 2026 to support organisations in implementing the statement and meeting their annual reporting requirements. Register here if you are interested in attending.
Speaking of webinars, it's encouraging to report that almost 300 people have already registered for our webinar on improving the quality of ethnicity data across the NHS, taking place on 2 December 2025. More details, including how to register, are further down in the bulletin.
Congratulations to all finalists and winners recognised at this year’s HSJ Awards, celebrating outstanding commitment, leadership and innovation across the health and care system. We extend particular congratulations to the shortlisted teams in the Innovation and Improvement in Reducing Healthcare Inequalities Award category, highlighting excellent work to improve access, outcomes and experience for underserved and marginalised communities. The winner, Wiltshire Integrated Care Alliance – Well Farmers for Wiltshire (part of the NHS Bath and North East Somerset, Swindon and Wiltshire integrated care group), was commended for its collaborative, community-based approach to supporting farmers’ physical and mental health, reducing barriers to care and strengthening rural wellbeing. Well done to all involved for driving meaningful, impactful change.
With best wishes,
Dianne
Latest updates
The health of people in prison, on probation and in the secure NHS estate in England
A new report from the Chief Medical Officer highlights stark health inequalities for adults on probation, who start from poorer physical and mental health than the general population. Many face early-onset multi-morbidity, substance misuse and have a history of smoking. Despite high health needs, they encounter barriers to care – such as difficulties registering with a GP, digital exclusion and fragmentation between probation and NHS services.
The report calls for stronger partnership between probation, ICBs and local public health bodies to improve access and tailored prevention services.
First ever Men’s Health Strategy published on International Men’s Day
England’s first ever Men’s Health Strategy – a comprehensive plan to tackle the crisis in men’s physical and mental health and reduce inequalities - has been published by the Department of Health and Social Care.
Published on International Men’s Day (19 November), the strategy addresses the stark reality that men in England die nearly 4 years earlier than women on average, with suicide remaining one of the biggest killers of men under 50.
It supports the 10 Year Health Plan, particularly the shifts from sickness to prevention and from hospital to community.
Living with sickle cell disease and thalassaemia
Hear first-hand accounts in this video with Devesh and Hamza who share their personal experiences of living with sickle cell disease and thalassaemia and why they believe raising awareness is vital.
Devesh and Hamza were among the more than 100 patients and advocates who participated in an online event we hosted on 30 October 2025 to continue raise awareness of these conditions and reflect on the delivery of our Sickle Cell and Thalassaemia Improvement Programme.
The contributions of those who attended – including patients, families, carers and patient representative organisations – will help shape the priorities and delivery of our programme as we continue work to improve patient care.
Encourage patients to complete the National Cancer Patient Experience Survey
The 2025 National Cancer Patient Experience Survey (NCPES) has commenced, with fieldwork closing on 30 January 2026.
All adult NHS patients with a confirmed primary diagnosis of cancer who have been admitted to hospital as inpatients for cancer related treatment or who were seen as day case patients for cancer related treatment and have been discharged during the months of April, May or June 2025, will be sent a survey about their experience of cancer care.
An updated communications toolkit is available on the NCPES website to promote the survey. Please help raise awareness of the survey to encourage as many people as possible to complete the survey when they are invited to take part in November.
If you have any questions, please email cpes@pickereurope.ac.uk.
Health improvement training for Core20PLUS Connectors
In collaboration with the Royal Society for Public Health, we are pleased to announce that 12 free places are now available on a new health improvement training programme for Core20PLUS Connectors working across England.
This is part of a wider collaborative strategy to develop the capacity and capability in communities to tackle inequalities and improve health and wellbeing.
Click here to find out more and apply. The deadline for applications is 30 January 2026.
Hope, progress and accountability: Tackling racial inequalities in mental health together
In a blog to mark Black History Month and World Mental Health Day in October, Dr Jacqui Dyer, NHS England’s Mental Health Equalities Adviser, reflected on the ongoing mission to address racial disparities in mental health, highlighting the progress made, the shared accountability we hold and the importance of sustained collaboration as we move forward into a new era shaped by the 10 Year Health Plan and the upcoming Mental Health Bill.
Sara Javid wins APNA NHS Rising Star Award
Congratulations to Sara Javid, one of our Senior Programme and Policy Managers, who won the NHS Rising Star Award at last month’s Asian Professionals’ National Alliance (APNA) annual conference, recognising her leadership, advocacy and commitment to inclusive change in healthcare.
Sara also walked away with two outstanding contribution merits — APNA Hero and Impactful Equality, Diversity and Inclusion Champion.
APNA is supported by current and former NHS leaders, and its annual national conference and awards recognise excellence, strengthen leadership and helps accelerate action to reduce health and workforce inequalities.
News from our partners
English indices of deprivation 2025
The English indices of deprivation 2025 - an important tool for identifying the most deprived areas in the country - is now available here.
Local policy makers and communities can use it to ensure that their activities prioritise the areas with greatest need for services.
Health Inequality Assurance Framework: a self-assessment improvement tool for ICBs
This supportive tool, published this month by NHS Confederation, will help integrated care boards (ICBs) to capture progress against strategic objectives and commissioning plans to tackle health inequalities and improve outcomes for all.
New programme to tackle bullying, harassment and abuse in the NHS
The NHS Race and Health Observatory has announced a new 16-month programme aimed at closing the ethnicity gap in bullying, harassment and abuse claims in the NHS.
According to the latest NHS Workforce Race Equality Standard Report, in 2023, 89% of NHS hospital trusts reported a higher proportion of Black and minority ethnic staff compared to white staff experiencing harassment, bullying or abuse from staff in the last 12 months.
Boosting breast screening confidence
A new digital initiative is helping to improve breast screening uptake and reduce inequalities across mid and south Essex.
A short, patient-centred video explains the screening process step by step, helping women feel more informed and less anxious about attending screening appointments.
Local insight shows almost four in 10 eligible women in Thurrock and Southend miss their appointments, compared with three in 10 across Essex and England.
To make screening more inclusive, accessible and translated versions have been produced, alongside Let’s Talk About Breasts – a dedicated film for women with learning disabilities and autism. Find out more here.
Bradford Doulas: Empowering Bradford mums during pregnancy and early parenthood
For over 14 years, Bradford Doulas has supported vulnerable women and birthing people through pregnancy, birth and early parenthood, helping tackle inequalities and ensuring no one faces birth alone. Find out more about their work.
Events and webinars
Book your place at NHS ConfedExpo 2026
Registration is now open for NHS ConfedExpo, the UK's leading health and care conference, returning to Manchester Central on 10-11 June 2026.
Connect with key decision makers, explore innovative ideas, and discover how teams are turning the ambitions of the 10 Year Health Plan into a reality.
If you have a bold idea, pioneering project, or practical insight to share, submit a breakout session proposal and be part of shaping the 2026 programme. Find out more about the submission process here.
Book your place. NHS, local authority and public sector staff receive free tickets.
A message from Dr Dianne Addei, Director - National Healthcare Inequalities Improvement Programme, NHS England
As we approach the end of Black History Month, we have achieved an important milestone with the publication yesterday of our Ethnicity Recording Improvement Plan. The plan sets out our ambition to strengthen the quality, consistency and completeness of ethnicity data across the NHS.
It outlines targeted actions for NHS organisations to identify and act on issues with ethnicity data quality which impact on their understanding of, and ability to act on, inequalities experienced by patients and the population.
Good quality data – complete, accurate, up-to-date and recorded consistently across systems – is essential for effective service planning and delivery and ensuring services offer equitable access, experience and outcomes for all.
Research has shown that ethnic minority people report poorer healthcare experiences and outcomes, and poor quality ethnicity data makes it harder for the NHS to understand who is being left behind and why.
I would like to thank my team and all stakeholders who contributed to the development of this pivotal plan.
Earlier this month, I was part of a team of NHS England leaders who visited Cambridge to see one of the country’s first Probation Neighbourhood Health Services in action. The service, supported by our programme, is pioneering an integrated approach to healthcare for people on probation – a group that experiences starkest health inequalities.
Based in the Cambridge Probation Office and nearby Access Surgery, the service offers nurse-led health screening during probation appointments, with onward referral when needed, a dedicated health navigator to support people to access services and address complex needs, and data collection and evaluation by Anglia Ruskin University to inform future commissioning and ensure services meet real needs.
This neighbourhood model directly responds to the 10-Year Health Plan’s call for community-based, preventative care. It demonstrates how closer links between probation, health and wider community services can break down barriers and support rehabilitation.
If we do not tackle the health problems faced by people on probation systematically, we risk a long chain of preventable ill-health in the community. This new model shows how we can put policy into practice.
The visit highlighted both the challenges and the opportunities to build sustainable, joined-up healthcare solutions for people on probation, with the Cambridge pilot offering a vital blueprint for the future.
Thank you for all you continue to do to support our shared mission of reducing healthcare inequalities.
With best wishes,
Dianne
Latest Updates
Tackling racism including antisemitism
We are asking NHS leaders for assistance in implementing important initiatives that support our shared commitment to fostering an inclusive, respectful and professional environment – for colleagues, patients and visitors – across the NHS, and assuring our communities of our commitment to tackling hatred in all its forms.
We take a zero-tolerance stance to all forms of hatred, antisemitism, Islamophobia, racism and to any form of discriminatory behaviour. In line with this, we are formally and actively adopting the International Holocaust Remembrance Alliance working definition of antisemitism.
The government is also reviewing the recommendations of the independent working group on Islamophobia.
Speak up month: creating a culture of safety
We are dedicated to ensuring everyone working in the NHS feels safe, and supported, to speak up. We want the NHS to be the best place to work and the safest place to receive care.
As part of Speak Up month, we encourage healthcare leaders to explore our published resources that demonstrate compassionate and responsive action and supports effective speaking up arrangements here.
Improving diversity in health and care research
NHS trusts are invited to join a pilot project launched with the Department of Health and Social Care (DHSC) to improve our understanding of the diversity of people taking part in health and care research.
Working the National Institute for Health and Care Research (NIHR), the pilot will gather data to help the NIHR, NHS England and DHSC to assess how well research participation reflects the UK’s diversity – and identify where more action is needed.
Sickle cell disease: what every clinician needs to think about
A sickle cell crisis can present itself in different ways, making early recognition vital to ensure patients receive rapid, safe and effective care.
In a new blog, Dr Rossby Awadzi, a GP trainee and Sickle Cell Clinical Fellow at NHS England, discusses the varied presentations of a sickle cell crisis and why it is important to prioritise patients experiencing one. He also highlights the crucial role of emergency department bypass units in improving outcomes and delivering better, more timely care for people living with sickle cell disease.
Dietitian wins 2025 CAPHO Award for sickle cell nutrition service
Dr Claudine Matthews, a consultant dietitian at Shoreditch Park and City Primary Care Network, won the AHP Innovation and Improvement Award at this year’s NHS England Chief Allied Health Professions Officer (CAPHO) Awards, for developing the Sickle Cell Nutrition Academy, which addresses nutrition knowledge and care provision gaps, empowering patients to better self-manage their condition and improve their outcomes.
Claudine has been involved in the work of our Sickle Cell Disease and Thalassaemia Improvement Programme, sharing information and resources to improve the quality of nutrition services for sickle cell patients.
How acting as an anchor employer can help the NHS address health inequalities in coastal communities
Our Senior Policy and Programme Manager, Cicely Ryder-Belson, has written a blog, sharing key insights from her visit to Great Yarmouth’s Apollo Project, a two-year workforce programme that offers support for people looking to start a career in health and care.
Great Yarmouth is one of the 16 sites in the Coastal Navigator Network. Her blog shows how the NHS can have a dual role as an anchor employer, by helping to reduce health inequalities in coastal communities while also tackling economic inactivity.
Black History Month: Leadership and representation
This Black History Month, senior NHS London executives have been reflecting on why diverse leadership matters and how representation shapes the quality and equity of healthcare across the capital.
Read Professor Kevin Fenton's blog to hear his insights on leadership, inclusion and the steps we can take together to build a fairer, more inclusive NHS. Professor Fenton is the Director of Public Health for London at the Office for Health Improvement and Disparities.
News from our partners
Health information you can trust from the revamped PIF TICK website
The PIF TICK website has been updated to signpost users to more than 145 trusted information creators. Following workshops with staff in the NHS and public libraries, the Patient Information Forum has updated its online directory of information materials produced by organisations that meet the PIF TICK quality criteria.
The updated website makes it easier for the public to find information on different health topics. The PIF TICK is the UK's only quality mark for health information.
Improving health literacy in the NHS
This guide - produced in partnership with NHS England - explores what is meant by health literacy, the benefits of applying health literacy interventions, recommendations for NHS trust board members and case studies from five NHS trusts that have effectively embedded interventions.
Black History Month: free e-learning courses for healthcare professionals
Healthcare professionals can learn about specific healthcare issues affecting the Black community in two free e-learning modules.
'Diagnosing breast cancer in Black women' is available on the RCGP website for any healthcare professional to register for free.
It takes 30 minutes and explores the risk factors that affect Black women and potential barriers to diagnosis. Sign up for a free RCGP account here.
Also available is the sickle cell disorder national education programme, a comprehensive e-learning course focusing on improving clinical knowledge of sickle cell disease.
Simply register for a free account or log into on the NHS Learning Hub to get started.
Latest LeDeR report now available
The 2023 ‘Learning from Lives and Deaths – people with a learning disability and autistic people’ (LeDeR) report is now available online.
The report, presented to Parliament in September, reviews deaths in England for autistic adults and adults with a learning disability to provide learning for the future and improve care.
This latest report placed a greater focus on the deaths of people with a learning disability from ethnic minority backgrounds and the deaths of people with a severe or profound learning disability.
Events and Webinars
Join our Healthcare Inequalities Improvement Forum
Wednesday 19 November 2025 - 10:00 am - 11:30 am | Online
The Forum - which takes place monthly - is a national platform for health and social care professionals with a keen interest in reducing health inequalities, including colleagues working at regional and system levels in the NHS.
It aims to promote collaboration, facilitate shared learning and provide support across the NHS. It is instrumental in shaping health policy, identifying barriers, sharing good practice and enhancing the capacity of the system to achieve equitable health outcomes.
If you have any questions, please email england.healthinequalities@nhs.net
Launch of new ICB Health Inequalities Assurance Framework
Wednesday 19 November 2025 – 4:00 pm – 5:30 pm | Online
We commissioned NHS Confederation to develop a new Integrated Care Board (ICB) Health Inequalities Assurance Framework to ensure that tackling health inequalities is at the heart of the role of ICBs.
The framework will help ICBs measure their own progress against the five key national priorities on health inequalities, alongside the three shifts outlined in the 10-Year Health Plan.
Register to join the live launch of the framework.
You will hear from ICB leaders who were involved in developing the framework and why they think this tool is important for all ICBs.
Webinar on improving the quality of ethnicity data across the NHS
Tuesday 2 December 2025 - 2.00 pm - 3.30pm | Online
We have launched an Ethnicity Recording Improvement Plan to strengthen the quality, consistency and completeness of ethnicity data across the NHS.
Good data means better decisions. By recording accurate, complete and up-to-date information, we can plan services more effectively and make sure everyone receives fair access, experiences and outcomes.
The plan sets out practical steps for NHS organisations identify and address data quality issues, helping us better understand and tackle health inequalities.
To support the implementation of the plan, we are hosting a webinar that will set out our ambitions and expectations of ICBs and providers, share practical examples of improving ethnicity recording and support organisations to reflect on how they can improve ethnicity recording.
Please click here to register for the webinar.
Have you seen?
This Black History Month profile of Dionne, the Director of Nursing at the St George's, Epsom and St Helier Hospital Group, who followed in the footsteps of her aunt, Yvonne, who was part of the Windrush generation that came from the Caribbean to work in the NHS.
Other
The Whole System Approach to Healthy Weight grants programme for Gosport is now open. Grants of up to £4,999 are available for projects that align with local healthy weight priorities, themes and focus populations.
Applications are open to organisations that are recognised legal entities (e.g. charities, community or social enterprises, local authorities, schools).
Full details and how to apply can be found here.
A new interactive resource which has been a collaborative project between DHSC OHID, UKHSA, NHSE with representatives from local government, ICB and VCSE to support work on inclusion health at a local level. Its purpose is to support informed decision-making and develop tailored solutions to the specific challenges these groups encounter, especially in the context of implementing the 10 Year Health Plan for England: fit for the future, and advancing the integrated neighbourhood health offer.
It contains a summary of statistics already in the public domain and brings these together into one place with accompanying narrative to highlight the importance of addressing the needs of inclusion health groups across different organisations, sectors, and programmes of work. The populations included are:
- People experiencing homelessness
- Gypsy, Roma and Traveller communities
- Sex workers
- Migrants in vulnerable circumstances
- People subject to modern slavery
- People in contact with the justice system
- People experiencing drug and/or alcohol dependence
Access the dashboard here.
Treetops Sexual Assault Referral Centre (SARC) has a new location.
Join them for one of their open days on either Thursday 26 or Friday 27 February.
The new SARC address: Mariners House, Waterside Gardens, Fareham, PO16 8SD
Go and see the new building, updated facilities, meet the staff and learn more about the important work they do.
Three sessions will be are available for each day (9:00, 12:00, 14:00). Please pick one and arrive five minutes before the time.
Sign up here.
Connect 5 is an evidence-based course ideal for businesses, local authorities, charitable organisations and community groups as well as individuals working in key settings. The Connect 5 course helps to build the capacity and capability of people to have more proactive and supportive conversations about mental health, wellbeing and suicide.
FULLY FUNDED SPACES AVAILABLE – Havant and East Hants Mind can offer fully-funded places for anyone living, working or volunteering in the public or voluntary sectors, within Hampshire, Portsmouth and Southampton There is a possibility that they can also offer subsidised course places, even if you do not fit within the prerequisites above.
Find out more here.
In the past six months, the number of practices signed up to Safer Surgeries in Hampshire and the Isle of Wight has more than doubled, rising to 26 practices. This growing momentum reflects a shared commitment to making primary care safer and more accessible for everyone, especially patients who may face barriers to care.
Why sign up?
Becoming a Safer Surgery means joining a network of practices that are making small, practical changes to reduce health inequalities. You’ll receive guidance and tools to:
- Create a welcoming, non-discriminatory environment
- Support patients without documentation or with uncertain immigration status
- Tackle barriers to registration and care
The benefits are clear: improved patient trust, enhanced safety, and alignment with NHS core values of inclusivity and equity.
📩 To find out more visit Introduction to Safe Surgeries: Improving access to Primary Care
Let’s keep the momentum going – together, we can make every surgery a safer surgery.
Let’s Talk About Vaccines (LTaV) is a training session to help build your confidence, skills and knowledge to open up discussions with service users about vaccination decisions in your local area.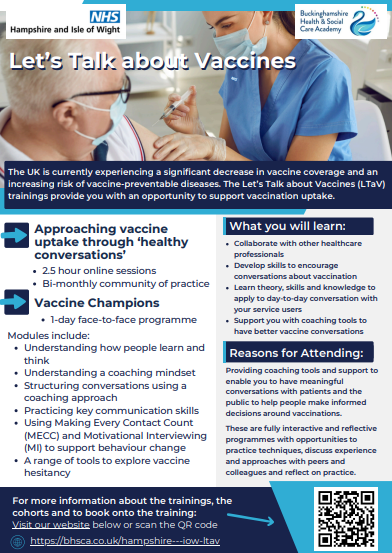
This 2.5-hour online, interactive session is free to health, social care and voluntary sector staff within the NHS Hampshire & Isle of Wight ICB footprint.
This training uses approaches from:
- Making Every Contact Count (MECC)
- Shared Decision Making
- Motivational Interviewing (MI)
Apply here.
The Active Practice Charter is an initiative by The Royal College of GPs and Sport England to inspire and celebrate the GP practices that champion the role of physical activity in improving everybody’s health and wellbeing. Become an RCGP Active Practice.
Become an Active Practice by making some simple but impactful changes that demonstrate to your patients and staff that movement is medicine, and we can all feel better by moving more. See here the practices that have already achieved their chartership RCGP Active Practice Charter map.
The Active Practice Charter is free to join; all you need to do is demonstrate you have taken steps in the practice to:
Reduce sedentary behaviour in staff and patients
Increase physical activity in staff and patients
Partner with a local physical activity provider
The initiative can be led by anyone in the practice, and aimee.cadman@energiseme.org from your local active partnership, offers tailored support for practices to achieve the accreditation – get in touch to discuss further.
The NHS Hampshire and Isle of Wight Improving Together platform offers everyone across Hampshire and Isle of Wight a repository of resources and tools that support continuous learning and improvement, including local and national training and development opportunities, links to join learning and improvement networks, and newsletters and bulletins you can subscribe to.
There is also an internal page on Stay Connected for ICB staff to access which is regularly updated with new training opportunities and improvement resources.
The Making Every Contact Count (MECC) train-the-trainer (TtT) course consists of two half days, and one full day of training. This will prepare you to deliver MECC training within your organisation, and beyond. The training is face-to-face and is not available online. Complete the application form and email to england.mecc.wx@nhs.net
The session will provide information about our service in Hampshire, outline our referral process and treatment options, as well as provide some basic drug and alcohol awareness training.
This session is aimed at professionals working with people who may benefit from drug and alcohol treatment/support, or staff members from our partner agencies who would like to expand their knowledge around drugs and alcohol.
Sign up now to the Nutrition Academy quarterly e-newsletter. You will receive the latest research, news and expert views on diet's crucial impact on lipid management and cardiovascular health.
Subscribe to stay informed and stay ahead with the leading experts in cholesterol management. You can unsubscribe anytime.