Personalised Care means people have choice and control over the way their care is planned and delivered, based on 'what matters' to them and their individual strengths, needs and preferences. This happens within a system that supports people to stay well for longer and makes the most of the expertise, capacity and potential of people, families, and communities in delivering better health and wellbeing outcomes and experiences.
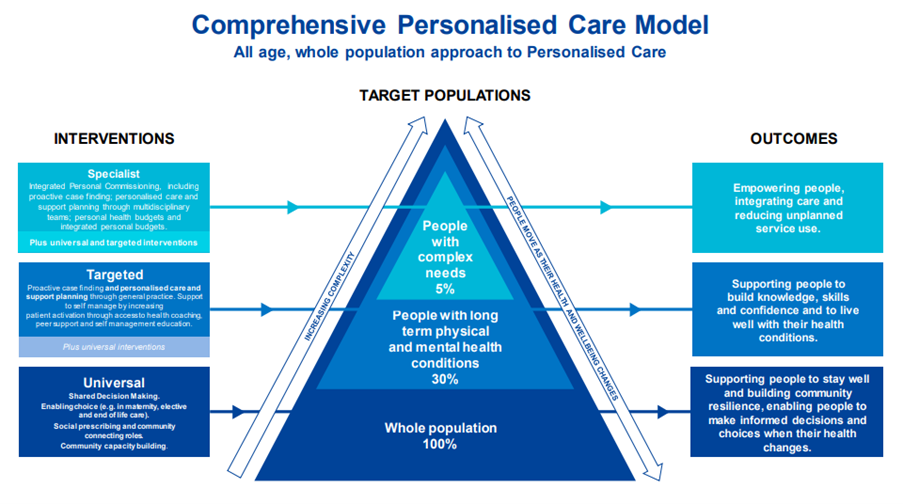
The Personalised Care Operating Model shows how all the various components work together to deliver a joined-up approach around the needs of each individual.
It is a legislative requirement of the Joint Forward Plan to promote patient involvement and each ICB should describe actions to implement the comprehensive model of personalised care.
This comprehensive model of care establishes whole population approaches to supporting people of all ages and their carers to manage their physical and mental health and wellbeing, build community resilience, and make informed decisions and choices when their health changes.
Personalised care and support planning is a series of facilitated conversations in which the person, or those who know them well, actively participates to explore the management of their health and wellbeing within the context of their whole life and family situation.
Developing a personalised care and support plan is a key component of Proactive Care. For further details on our ICB framework click here.
What Matters to You
As healthcare professionals, we want to promote careful, kind human interactions. Asking 'What matters to you?' is about understanding what matters to an individual in their life. It's about having meaningful conversations with individuals, as well as their families and carers. For further information visit: www.whatmatterstoyou.scot
Training
For free online accredited training visit: Personalised Care Institute
Shared decision-making ensures that individuals are supported to make decisions that are right for them. It is a collaborative process through which a clinician supports a patient to reach a decision about their treatment.
Decision Support Tools
These decision support tools are designed to support shared decision making between people and a clinician.
Good Practice Examples
Social prescribing is a key component of personalised care. It is an approach that connects people to activities, groups, and services in their community to meet the practical, social, and emotional needs that affect their health and wellbeing.
Hampshire and Isle of Wight Social Prescribing Network
Coordinated by Community First, the Hampshire and Isle of Wight Social Prescribing Network was established in 2017. There are three free Webinars and one face to face networking and showcase meeting per year, as well as interim Social Prescribing updates and news. The Network is funded by Hampshire and Isle Wight Integrated Care Board and has c400 members who deliver, commission, or provide services for or support social prescribing projects countywide.
To register or for more informaition contact Jane via healthforums@cfirst.org.uk or 07917718409.
Social Prescribing Link Worker Map
South East Thriving Communities Team is working with social prescribing leads from the NHS to develop the Social Prescribing Link Worker Map for the region. This mapping project seeks to improve community connections with social prescribers by making it clear where link workers are located.
NASP
NASP is a national charity that champions social prescribing. They support and connect people, communities, and organisations so that more people across the UK can enjoy better health and wellbeing.
ICP Social Connectedness Framework
Social connection between people is important for physical and mental health and contributes to an improved quality of life. The ICP Social Connectedness Framework developed by Hampshire and Isle of Wight Integrated Care Partnership aims to increase understanding of social connectedness and support local 'place' plans to reduce social isolation.
Supported self-management means increasing the knowledge, skills and confidence a person has in managing their own health and care.
Healthy Hearts
There are a lot of different resources and information out there to help people keep their hearts healthy. Visit the Hampshire and Isle of Wight ICB Healthy Hearts page for more information tailored to patients and professionals.
Peer Leadership Programme
The Peer Leadership Programme is a personal development programme for people with living experience and is delivered online via an accessible and interactive learning platform called Future Learn.
Blood Pressure Checks
Video from NHS England to promote blood pressure checks.